Trending Post
Telehealth: Its Past, Present, and the Future
Mohamed Vaseem
Before the COVID-19 pandemic, telehealth was a crucial topic when debating the future of healthcare. But during the pandemic, with physical distancing and stay-at-home orders in place, telehealth had become a necessity for many. Today, almost every healthcare environment and field of specialty transfer patient information and health data for distinctive purposes.
Telehealth blends physical and digital for effective, trusted, and reliable care that meets people where they are and delivers what they need. Like any customer-oriented solution, telehealth focuses on continually improving patient care and experience.
With the ongoing hustle to find better ways to treat patients, all innovations that will become the standard for remote healthcare in the future will have a common goal – to provide seamless and comprehensive medical services to patients irrespective of their location or situation. From extending the services in rural regions to enhancing the availability of care during pandemic times, telehealth has blurred the boundaries and sacked the barriers.
A brief about telehealth
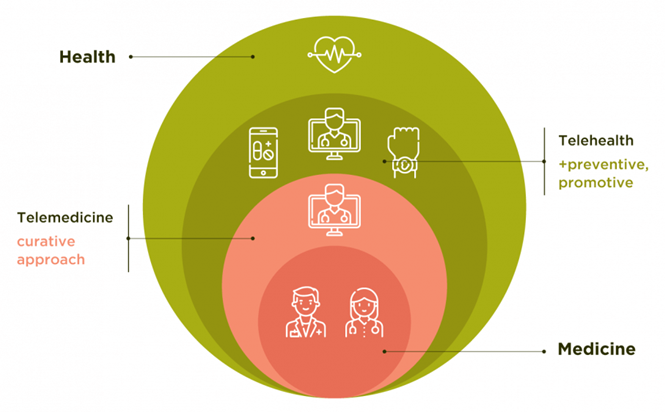
Telehealth refers to a broader spectrum of remote healthcare services that uses electronic information and telecommunication to support remote clinical health care, patient and professional health-related education, public health, and health administration.
Telehealth Services
Telehealth service includes Synchronous visits, Asynchronous communication, Remote Patient Monitoring (RPM), and Mobile health (mHealth).
Synchronous visits refer to a real-time two-way conversation between patients and their healthcare providers. It can include various treatment types, such as primary care visits and pharmacy consults for medication reviews.
Asynchronous virtual care means transmitting information through methods like patient portals and secure emails, where communication does not happen simultaneously.
Remote patient monitoring is a method of sharing real-time patient data to a provider for clinician to monitor a patient's chronic conditions from a different location.
Mobile health is to support ongoing healthcare through mobile appliances such as laptops, smart watches, and iPhones with safety-based software applications.
The past, the present, and the future
Telehealth before COVID-19
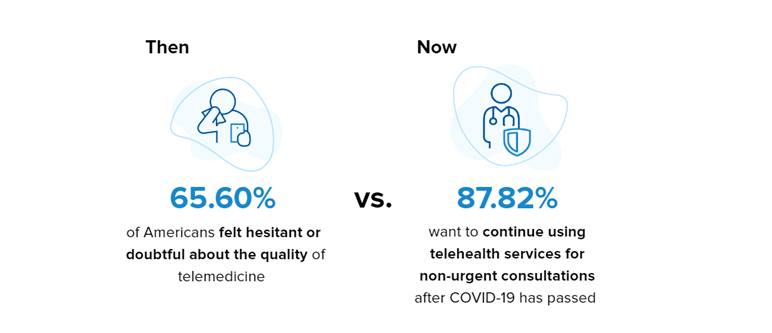
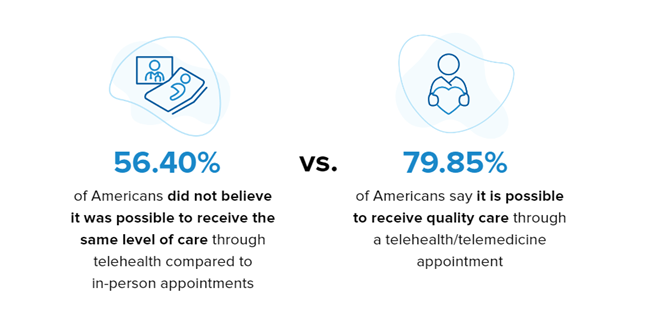
Telehealth existed long before the COVID-19 pandemic, i.e., its existence can be dated back to the 1960s but on a much different scale. Before COVID-19, the consumers didn't think telehealth would give them comparable care to in-person visits.
Virtual care options were not trusted back then. Both patients and providers questioned the reliability.
Most believed it to be impersonal and would not lead to long-lasting relationships. It was the 2016-2019 period that witnessed a lift and shift in virtual health appointments.
Various studies showed steady growth in the number of virtual health appointments, and a significant number of clinicians agreed that it would continue to increase steadily in the future.
Telehealth during COVID-19
With the imposition of lockdown in every part of the world, everything turned virtual. Regular health check-up appointments were canceled or put on hold. But for a fact, care can't be and must not be delayed. Virtual appointments then became the savior. By March 2021, an estimated 61% of consumers had virtual care appointments, which was estimated 19% in March 2020. The deficiency exists no more. Consumers can now timely book appointments and save time and cost with virtual mode.
The future of telehealth - Becoming a saving grace
Increased consumer utilization
The pandemic has accelerated telehealth utilization, making it more than 38 times that of pre-pandemic. With the increased acceptance of virtual care among patients, telehealth is going to witness a continuous rise in usage. As per a survey conducted by McKinsey, more than 75% of the patients said they would use telehealth in the future.
Advanced chronic care management
On a global level, about 1 in 3 adults suffer from chronic conditions, including obesity, kidney disease, cancer, asthma, alzheimer's disease, diabetes, and stroke side effects. Telehealth is a convenient mode for patients to connect with their doctor in less time and at regular intervals. They don't have to go through long waits in the waiting rooms and bear the expanses of commute to the doctor's office.
Prioritize and focus on mental health
According to the World Health Organization, Corona virus outbreak resulted in disrupted mental health services in 93% of countries globally.
Many healthcare professionals, therapists, and doctors turned to video conferencing to continue treating and supporting patients and maintaining continuity in the care delivery cycle. Hence the development of teletherapy and telepsychiatry started, and it is likely to become a widely accepted form of treatment in the coming times.
Improved patient experience
Patients don't want to juggle multiple apps and websites; they want their telehealth experience to be efficient, seamless, and integrated. This increases pressure on developers to look for ways and ideas to ensure comprehensive service through integrated communications such as video, calls, webchat, and bots.
Some emerging use cases include real-time health updates, timely reminders of follow-up appointments, etc. In addition, the information and data must be simplified for easy use so that patients can access and navigate at the touch of a button without any hassle.
Integrated data exchange
The concept of integrated data exchange is induced by interoperability. Interoperability signifies the ability to access, share, integrate, and cooperatively utilize the data within and across various organizations. Interoperable systems not only transmit or share the data but can interpret, preserve its actual context, and present it as it is obtained.
Remote patient monitoring & wearable technology
With telehealth becoming critical for people with chronic conditions and the uptake of integrated data exchange, wearable technology has become the trend. Wearable technology has spread its roots far and wide with improved development and growth in sales of smart watches and fitness trackers.
The healthcare industry took up and had efficiently begun remote patient monitoring. Wearable devices allow doctors to track their patient's day-to-day activity and gather real-time data on several health measures such as heart rates, blood pressure, sleep cycles, and more.
According to research, the global telehealth market is projected to reach USD 285.7 billion by 2027, at a CAGR of 26.6%.
The global telemedicine market anticipates growth from USD 41.63 in 2019 to USD 396.76Bn in 2027 at a CAGR of 25.8%.
Limitations to be aware of
Telemedicine definitely has its strong points bringing gauging health benefits, but there are some limitations that also have to be considered.
Internet connectivity
Telehealth services heavily depend on a stable and fast internet connection, and it's possible not every patient has it. The major limitation to telehealth is that if the patient or physician/doctor/health experts lose connectivity, the appointment cannot be completed, leading to delays and even postponement, further hindering other scheduled visits.
Smart devices
To support telehealth services, patients and doctor/health experts are not only required to have an uninterrupted and speedy internet connection but also smart devices that support the necessary applications. Healthcare practice will have smart devices, but if the patients don't, they simply won't be able to access any services.
Generation gaps
The youngsters have no trouble dealing with technology. It is rather convenient and time-saving considering their fast-paced lives. On the contrary, the experience differs for older generations due to inexperience using technology or, in some cases, because of physical disability. Elderly patients face multiple problems operating these devices, understanding the functionality, and making proper utilization of such services.
Patient data safety
Patient information is subjected to security risks while conducting the appointments online. Telehealth service providers must consider data safety measures and prevent patient information confidentiality.
Conclusion
Telehealth services are not a full-fledged substitute for in-person visits, but it has proven to be highly convenient for patients. Its surprising benefits are yet to be realized in public health, improving access to quality care, minimizing financial stress, and easing pressure on healthcare professionals.
There is plenty we can't comprehend yet about the future of telehealth. Still, as its use rapidly expands and we prepare for the future, we can all agree that telehealth must be safe, effective, efficient, timely, equitable, and patient-centered.
Of course, some obstacles may delay the integration process between traditional healthcare and telehealth. Hospitals need the right technical infrastructure; governments must think about legalities; doctors should rethink ethics and find ways to accurately diagnose their patients without the ability to touch them or look closely. Still, most researchers agree that telehealth has a bright future.